Otitis Externa and Otinova: A Practical, No-Nonsense Guide If your ear suddenly feels itchy, sore, blocked, or painful after swimming or showering, you may be dealing with otitis externa —often called “swimmer’s ear.” The good news: most cases are very treatable with the right early steps. This guide explains what otitis externa is, why it happens, where Otinova fits in, and when to escalate quickly. What is otitis externa? Otitis externa is inflammation (and sometimes infection) of the skin lining the external ear canal. It commonly presents with: Ear pain (often worse when touching or pulling the outer ear) Itching Fullness/blockage Reduced hearing from swelling/debris Sometimes watery discharge Otinova’s own instruction documents describe it as treatment for ear canal inflammation/eczema (swimmer’s ear). Why does it happen? The ear canal is protected by a mildly acidic environment and a skin barrier. Otitis externa tends to flare ...
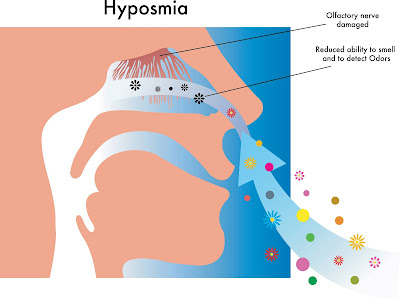
What causes loss of smell?
Sense of smell is vital to us. Loss of sense of smell is most commonly due to a cold or flu. Patients who suffer from sinus infections or hay fever can have intermittent loss of smell. In some cases, due to growth, such as nasal polyps or, in rare cases, a tumour can affect the sense of smell. These conditions can either lead to a total loss of smell, reduced sense of smell, altered smell or a sensation of smell when it is not there.
Why do we lose the sense of smell in COVID-19 or Coronavirus infection?
Coronavirus has been well-known to cause flu-like symptoms. COVID 19 is a type of coronavirus, so WHO has stated loss of smell as a possible symptom of COVID 19. In some cases, COVID-19 infection can affect nerve endings, resulting in Anosmia symptoms. Return of sense of smell depends on how these nerve endings regenerate.
Should I be worried about the loss of sense of smell?
The loss of sense of smell can be due to COVID infection. There can be other causes which can lead to loss of smell and taste. If your symptoms persist after COVID infection has resolved, you should seek advice from ENT surgeon to offer you medical treatment.
How be loss of smell cured?
As smell fibres are present right at the top part of our nose, using medical treatment can help improve your symptoms. To prevent the spread of COVID infection, you should first book a telephone consultation with your GP, Pharmacist or ENT surgeon.
Initial management includes sinus rinse to cleanse your nose with or without the use of steroid nasal spray. You can get these medications delivered to your doorstep.
What is safety advice for people with loss of smell?
Gas safety is vital if your sense of smell is altered. Regularly check your safety alarm. Get gas servicing routinely done.
You may not be able to smell food, so always check for use by date and always ask others to smell food for and look for visual clues for rotten food. As you cannot smell yourself, maintain constant good body hygiene.
What can I do if my sense of smell does not come back?
It is vital to seek advice and examination by ENT surgeon if your sense of smell does not come back. ENT surgeon with a careful history, examination and nasal endoscopy may be able to advise you medical treatment. Failing trial of medical treatment, patients can undergo smell training.
Smell training is retraining your residual nerve endings to start working again. There is strong evidence that it does work in the vast majority of patients. It is like physiotherapy of nerve endings, so the results are slow. Smell training can be offered to patients who have lost sense of smell due to hay fever, flu, head and injury or COVID infection.
Helping Patients with Specialist Expertise and Kindness
Mr Gaurav Kumar
Consultant Ear Nose Throat Surgeon
Book an appointment
entsurgeonclinic@gmail.com
079494914140
Disclaimer: For general information only, always seek medical advice from treating consultant